Blastocyst transfer program
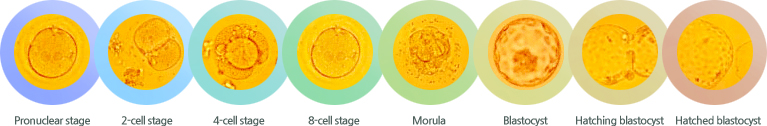
A blastocyst is a highly differentiated and developed embryo that has grown to the point, where it is ready to attach to the uterine wall (implantation). In natural pregnancy, the oocyte is released from the ovarian follicle and picked up by the fallopian tube, where it is fertilized by sperm. As the embryo grows, it undergoes cleavage, where the cell divides into smaller cells called blastomeres. After 2days, the embryo will consist of 4~8 blastomeres and after 3days, it will consist of 12~16 blastomeres. At this stage, the cells begin to compact, forming a morula, and the embryo enters the uterus. Finally, after 4~5days, the blastocyst is created.
- We can select healthy embryos by extending culture period. By watching the embryo's development to the blastocyst stage, the embryologists can have a better idea of which embryos are most likely to be healthy and continue to develop.
- We routinely transfer only two or three blastocysts to decrease the risk of multiple pregn ancy without lowering the chance that a patient will become pregnant.
- In blastocyst stage, the size of each cell is smaller and the number of cells is much more than in cleaving stage. So, the survival rate is much higher in blastocyst stage than in cleaving stage after cryopreservation.
Developmental stage of embryo
Media (YS medium)
YS medium was originally formulated according to the physiological condition of the female reproductive tract. We use the YS medium in the IVF program because it improves embryo development in vitro and prevents loss of embryo viability, which resulting in a higher implantation and pregnancy rates.
Media Quality Control
The culture medium, used for clinical IVF, was completely confirmed by animal test. All of our medium supplements were provided by several companies after careful screening. Also, all reagents were tested for the absence of cytotoxicity, endotoxin, and for the ability of growth promotion.
Coculture with cumulus cells
Cumulus cells, which are sometimes referred to as "feeder" cells or "helper" cells, stimulate development of the embryos by removing toxins from the medium and adding growth factors. Some studies and our results have demonstrated the improvement of pregnancy and delivery rates with utilization of coculture.
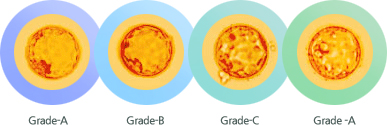
Morphological grading of the blastocyst
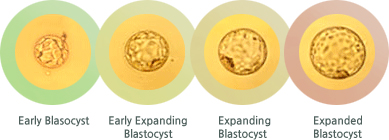
Extended culture of human embryos seemed to increase the discrimination of potential embryonic viability, with morphological criteria. Before implanting the Blastocyst, the last stage embryo, into the uterine wall, it will be differentiated into inner cell mass and trophoectoderm cells. We have classified blastocysts from A to D based on the morphological characteristics and the developmental rate. The grade A blastocyst has a high probability of pregnancy.
-
<The grade of blastocyst>
-
<Developmental stage of blastocyst>
Blastocyst cryopreservation
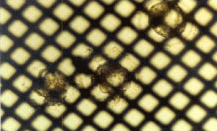
<Vitrification Using EM-grid>
In case of patients having supernumerary blastocysts after embryo transfer or having the risk of ovarian hyperstimulation syndrome, blastocysts can be frozen and stored in liquid nitrogen at -196℃ for decades. The blastocysts can be thawed at a later date and transferred to the uterus in a menstrual cycle with little or no premedication, providing additional opportunity for increasing cumulative pregnancy rate.
Assisted Hatching (AH)
Assisted hatching is a procedure that increases the chance of embryo implantation. The embryo must break out (hatch) out of the zona pellucida to implant in the uterus. One potential explanation for the failure of implantation is that the embryo did not hatch from the zona pellucida. Assisted hatching is a procedure that weakens (thinning or dissection) the zona pellucida prior to transferring the embryos into the uterus. This should help the embryos to hatch.
Intracytoplasmic sperm injection (ICSI)
ICSI is useful for male factor infertility, which includes oligozoospermic, asthenozoospermic, teratozoospermic, and for poor fertilization with conventional insemination. ICSI involves the insertion of a single sperm directly into an egg obtained from the ovary of a woman undergoing in vitro fertilization.
Percutaneous Epididymal Sperm Aspiration (PESA) & Testicular Sperm Extraction (TESE)
Sperm maturation (=spermatogenesis) takes about 60-70 days, in general. Spermatozoa, produced in seminiferous tubules, moves from the basal lamina towards the lumen, and then, to the ejaculatory ducts. When there is any problem during this process, PESA or TESE may be suggested. PESA is indicated for men with irreparable obstruction resulting in azoospermia and congenital absence of the vas deferens or who have had vasectomies or failed vasectomy reversals. The sperm are obtained directly from the epididymis or the vas deferens. TESE is available for men with infertility like spermatogenic arrest or testicular atrophy that cannot be treated by any other method. The sperm are obtained directly from the testis. In these cases, obtained sperm are fertilized with ICSI.
Round spermatid Injection (ROSI)
This method can be applied to azoospermia with complete spermatogenic arrest, derived from genetic defects or endocrine disorders. ROSI is the procedure in which the round(immature) spermid is injected into the oocyte when mature sperm cells are not obtainable. Although animal studies show high pregnancy rates with ROSI, limited studies in humans still indicate very high rates of embryo failure.
IVM/F ET program using immature oocyte
It is a very useful method for PCO patients who are prone to develop OHSS in response to gonadotropins. Immature oocytes are picked up in natural cycle without any stimulation, so there are no side effects in IVM/F-ET program. Collected immature oocytes are cultured in our specialized medium for maturation. This method is very simple and the cost is not expensive. The pregnancy rate is similar to that of standard IVF cycles, but we applied this program to limited patients.
Preimplantation Genetic Diagnosis (PGD)
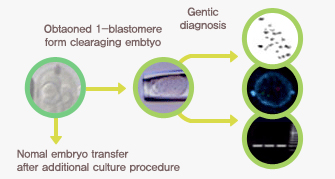
<Gentic diagnosis>
Preimplantation genetic diagnosis (PGD) enables physicians to identify genetic diseases of the embryos prior to implantation and before pregnancy is established. It's primary purpose is to select normal embryos. PGD was developed for patients who were at risk of having children with serious genetic disorders
Oocyte Cryopreservations
The cryopreservation of oocytes or ovarian tissue would provide additional help for women with serious diseases who want to preserve fertility after surgery, chemotherapy, or radiotherapy and for women wanting to delay maternity for any other reasons. However, only a few successful pregnancies have been reported with cryopreserved human oocytes. This situation has been primarily attributed to poor survival, fertilization, and development of cryopreserved oocytes, but we have developed other cryopreservation methods which increase the survival rate and developmental competence of thawed human oocytes.
Introduction of the up to date medical equipment to
improve pregnancy rates.
Maria Fertility hospital has introduced the latest medical equipment to improve pregnancy rates. We strive to assist infertile couples to build new families through endless researches on the fertility treatment. Thank you.
EmbryoScope Time-lapse system
Embryoscope Time-lapse System is the state-of-the-art technology, recently introduced in the United States and Europe. The principle of this equipment is to prevent the embryos from exposure to outside environment until embryo transfer while recording every step of the development of the embryos and selecting the top quality embryos.
It is highly expected that we can minimize the number of embryos transferred and improve pregnancy rates by using EmbryoScope Time-laps system.

(IMSI: Intracytoplasmic morphologically selected sperm injection)
The embryologist uses an extremely high-powered microscope (6600-times magnification) to select the sperm cells with the best morphological quality to be injected into the eggs, thereby increasing the probability that these sperm cells will fertilize the eggs.
In the sperm cells that may appear normal on the general ICSI, tiny defects in the head of the sperm can be detected using IMSI.